Highlights of our Work
2024 | 2023 | 2022 | 2021 | 2020 | 2019 | 2018 | 2017 | 2016 | 2015 | 2014 | 2013 | 2012 | 2011 | 2010 | 2009 | 2008 | 2007 | 2006 | 2005 | 2004 | 2003 | 2002 | 2001
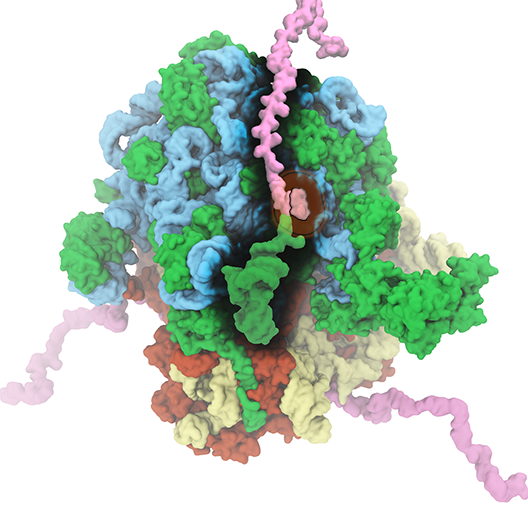
image size:
816.0KB
made with VMD
The ribosome is the ubiquitous machine in all living cells responsible for
translating the cell's genes into functional proteins.
The majority of antibiotic drugs target the ribosomes of bacterial cells while
leaving human ribosomes unharmed.
An example are the most widely-prescribed antibiotics, erythromycin and telithromycin.
They kill bacteria by changing the properties of bacterial ribosomes and, thereby,
disturb the bacterial protein production (see the Oct 2014 highlight Antibiotic Action on the Ribosome).
However, modern bacteria fight antibiotic drugs;
exposing them to a specific kind of antibiotic drug for too long will
trigger the expression of drug-resistance genes, which protect the bacteria,
eventually making the drug useless.
Due to historical overuse of antibiotic drugs,
clinic antibiotic drugs have experienced today serious drug-resistance problems.
In a joint effort of computational and biomedical investigations, reported recently,
molecular dynamics simulations with NAMD and systematic mutation experiments showed that
the above antibiotics interact in a bacterial ribosome with a drug resistance
gene - coded nascent protein and make it stall translation; however, engineered
simple mutations in the bacterial gene can abolish stalling and, thereby,
prevent the effect of drug resistance genes.
The research suggests that engineered mutations might be a strategy to prevent
antibiotic resistance.
Read more on our Ribosome website.